Flumazenil is a medication widely used in emergency medicine and anesthesiology. Known as a benzodiazepine antagonist, it is primarily used to reverse the sedative effects of benzodiazepines in clinical settings. Flumazenil is considered a vital tool in managing benzodiazepine overdoses, aiding in rapid awakening from sedation, and assisting in diagnosis of altered mental states caused by benzodiazepine toxicity.
In this article, we will explore the following aspects of Flumazenil in detail:
- What is Flumazenil?
- How does Flumazenil work?
- Clinical uses
- Dosage and administration
- Side effects and risks
- Contraindications and precautions
- Role in benzodiazepine overdose
- Drug interactions
- Summary and clinical considerations
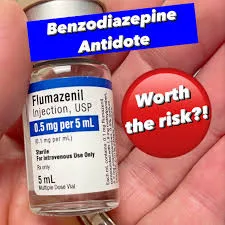
What is Flumazenil?
Flumazenil, marketed under brand names such as Romazicon, is a selective benzodiazepine receptor antagonist. It is used intravenously to reverse the sedative effects of benzodiazepines such as diazepam, lorazepam, midazolam, and others.
Basic Information:
- Drug class: Benzodiazepine antagonist
- Route of administration: Intravenous (IV)
- Onset of action: 1–2 minutes
- Half-life: 40–80 minutes
- Pregnancy category: C (use with caution)
Mechanism of Action
Benzodiazepines exert their sedative, anxiolytic, anticonvulsant, and muscle relaxant effects by enhancing the activity of gamma-aminobutyric acid (GABA), an inhibitory neurotransmitter in the central nervous system. They bind to the benzodiazepine site on the GABA-A receptor, increasing the frequency of chloride channel opening and causing neuronal inhibition.
Flumazenil works by competitively inhibiting the benzodiazepine binding site on the GABA-A receptor. It does not activate the receptor but prevents benzodiazepines from exerting their effects, effectively reversing sedation and other symptoms associated with benzodiazepine use or overdose.
Clinical Uses of Flumazenil
Its primary indications include:
Reversal of Benzodiazepine Sedation:
Used to reverse excessive sedation after diagnostic or therapeutic procedures, especially in surgical patients given benzodiazepines for anesthesia or conscious sedation.
Management of Benzodiazepine Overdose:
It can temporarily reverse the central nervous system depression caused by acute benzodiazepine toxicity.
Diagnostic Aid:
Helps differentiate benzodiazepine-induced unconsciousness or altered mental state from other causes, such as coma or neurological injury.
Dosage and Administration
Flumazenil is administered only via intravenous (IV) injection and must be given slowly to minimize the risk of adverse effects.
Typical Dosing for Sedation Reversal:
- Initial dose: 0.2 mg IV over 15 seconds
- If desired level of consciousness not achieved, additional 0.2 mg doses may be given every 60 seconds
- Maximum total dose: 1 mg (usually effective)
For Benzodiazepine Overdose:
- Start with 0.2 mg IV
- Titrate in 0.3 mg to 0.5 mg increments at 1-minute intervals
- Max cumulative dose: 3 to 5 mg
Note: Effects are rapid, but may be short-lived due to the short half-life of Flumazenil.
Side Effects of Flumazenil
Flumazenil is generally well-tolerated but can cause various side effects. These include:
Common Side Effects:
- Dizziness
- Nausea and vomiting
- Headache
- Agitation
- Fatigue
Serious Side Effects:
- Seizures (especially in patients with long-term benzodiazepine use or co-ingestion of tricyclic antidepressants)
- Cardiac arrhythmias
- Panic attacks in patients with anxiety
- Withdrawal symptoms in benzodiazepine-dependent individuals
Contraindications and Precautions
Flumazenil is not suitable for all patients, especially those with chronic benzodiazepine use or co-ingestion of drugs that lower the seizure threshold.
Absolute Contraindications:
- Known hypersensitivity to Flumazenil
- Seizure-prone patients (especially with tricyclic antidepressant overdose)
- Chronic benzodiazepine users (risk of withdrawal and seizures)
- Patients with intracranial pressure or head injury (may affect cerebral blood flow)
Precautions:
- Use with caution in liver impairment (prolonged effect)
- Monitor continuously after administration due to risk of re-sedation
Role in Benzodiazepine Overdose Management
Flumazenil can be life-saving in cases of isolated benzodiazepine overdose, especially when respiratory depression is present. However, its use is controversial due to risks associated with:
- Polysubstance overdose (e.g., TCA + benzodiazepine): Flumazenil may unmask cardiotoxicity or seizures
- Physical dependence: Abrupt antagonism can cause withdrawal seizures
- Short half-life: Symptoms of overdose may return after Flumazenil wears off
When to Use in Overdose:
- Known isolated benzodiazepine overdose
- No history of seizure disorder
- No long-term benzodiazepine use
- No co-ingestion of pro-convulsant drugs
In most emergency settings, supportive care (airway management, oxygen, fluids) is the first-line treatment, and Flumazenil is reserved for selected cases.
Drug Interactions
Flumazenil may interact with the following:
- Benzodiazepines: Antagonizes their effects
- Tricyclic antidepressants: May precipitate seizures
- Alcohol or barbiturates: Limited efficacy; does not reverse non-benzodiazepine CNS depressants
It’s crucial to determine all substances ingested before administration.
Clinical Considerations and Monitoring
After administering Flumazenil, continuous monitoring is essential:
- Observe for at least 2 hours post-administration
- Monitor respiratory rate, oxygen saturation, and mental status
- Be prepared to re-dose or initiate alternative treatments if symptoms recur
- Have anticonvulsants (e.g., benzodiazepines, ironically) available in case of seizure
Conclusion
Flumazenil is a powerful and selective benzodiazepine antagonist that plays a critical role in reversing benzodiazepine sedation and treating overdose in carefully selected patients. It acts quickly but has a short duration, requiring careful monitoring and often repeat dosing.
Though highly effective, Flumazenil should not be used indiscriminately, especially in patients with long-term benzodiazepine use or co-ingestion of other CNS depressants. The decision to administer Flumazenil should always be based on a thorough patient assessment and clinical judgment.
For healthcare providers, understanding the indications, risks, and proper use of Flumazenil is crucial for ensuring patient safety and successful outcomes in emergency and perioperative care.