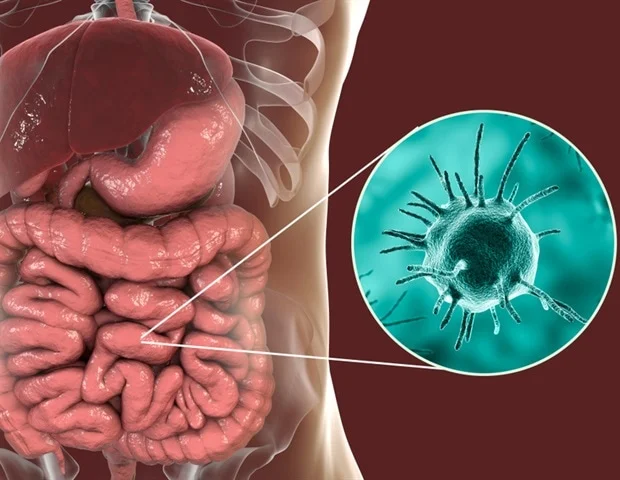
Intestinal amoebiasis, also known as amebic dysentery, is a parasitic infection caused by Entamoeba histolytica, a protozoan that primarily affects the large intestine. This infection remains a major health concern in developing regions, particularly where sanitation is poor and access to clean water is limited.
While intestinal amoebiasis can range from mild to severe, its effects on digestive health can be long-lasting if not properly treated. Understanding its causes, symptoms, diagnosis, treatment, and prevention is essential for both healthcare providers and the general public.
Understanding Intestinal Amoebiasis
Intestinal amoebiasis results from ingestion of E. histolytica cysts through contaminated food or water. Once inside the human digestive tract, the cysts transform into trophozoites the active form of the parasite which invade the intestinal lining, causing inflammation, ulceration, and in severe cases, tissue necrosis.
This process can lead to dysentery, abdominal pain, and nutrient malabsorption. The parasite can also travel beyond the intestines, infecting the liver and other organs, leading to amoebic liver abscesses. Because symptoms often resemble those of other gastrointestinal infections, proper diagnosis is essential to ensure effective treatment.
Symptoms and Clinical Manifestations
The symptoms of intestinal amoebiasis vary depending on the severity of the infection and the host’s immune response. Common manifestations include
- Abdominal cramps and pain
- Frequent loose stools or diarrhea, sometimes with blood or mucus
- Fever and fatigue
- Loss of appetite and weight loss
- Dehydration, particularly in severe cases
In chronic infections, patients may experience intermittent diarrhea, abdominal bloating, and prolonged nutritional deficiencies due to impaired absorption of nutrients. Over time, the infection may cause significant inflammation and ulceration of the colon, resulting in long-term digestive complications.
Impact on Digestive Health
The digestive system’s primary role is to absorb nutrients and eliminate waste efficiently. Intestinal amoebiasis disrupts this delicate balance in several ways:
Intestinal Inflammation and Ulceration
The parasite erodes the intestinal mucosa, forming ulcers that bleed and cause pain. This can lead to chronic inflammation and scarring in the colon.
Malabsorption of Nutrients
Damaged intestinal linings cannot absorb essential nutrients such as iron, vitamin B12, and proteins effectively. This often leads to anemia, weight loss, and general weakness.
Altered Gut Microbiota
Repeated or prolonged infections can disturb the balance of beneficial gut bacteria, increasing vulnerability to other gastrointestinal infections and inflammatory bowel conditions.
Digestive Irregularities
Persistent diarrhea and abdominal cramps can disrupt normal bowel movements, leading to dehydration and electrolyte imbalances.
These effects can severely impact an individual’s overall health, productivity, and quality of life, particularly in communities where repeated exposure is common due to inadequate sanitation.
Diagnosis and Clinical Evaluation
Accurate diagnosis is critical for effective management of intestinal amoebiasis. Laboratory tests play a central role, including:
- Microscopic stool examination: Detects cysts or trophozoites in fecal samples.
- Antigen detection tests: Identify E. histolytica-specific proteins in stool or blood.
- Serological tests: Useful in distinguishing between active and past infections.
- Imaging techniques (ultrasound, CT scans): Recommended for suspected extra-intestinal infections, such as liver abscesses.
Early detection not only improves treatment outcomes but also helps prevent transmission within communities.
Treatment Options
Treatment of intestinal amoebiasis involves eliminating both the active trophozoites and the dormant cysts to prevent recurrence. Commonly used medications include
- Metronidazole or Tinidazole: Effective against the active trophozoite stage.
- Paromomycin or Diloxanide furoate: Target cyst forms to prevent relapse.
- Supportive therapy: Includes rehydration, electrolyte replacement, and nutritional support.
While metronidazole remains the first-line treatment, in regions with mixed parasitic infections, broad-spectrum antiparasitic agents like mebendazole may be used to treat co-infections involving intestinal worms. This has led to increased demand for mebendazole wholesale distribution, particularly in public health campaigns aiming to control multiple parasitic diseases simultaneously.
The Role of Mebendazole in Parasitic Control
Mebendazole is a well-known anthelmintic medication that targets various intestinal worms, including roundworms, whipworms, and hookworms. Although it is not the primary drug for amoebiasis, it is often included in community health initiatives due to its effectiveness against coexisting parasitic infections.
Public health authorities and non-governmental organizations (NGOs) frequently procure mebendazole wholesale to ensure affordable access for deworming programs. By combining mebendazole with amoebiasis-targeted treatments like metronidazole, healthcare systems can address a broader range of parasitic infections that collectively burden digestive health in low-resource settings.
Wholesale access to such medications is crucial for cost-effective treatment distribution in hospitals, clinics, and humanitarian relief efforts. Reliable mebendazole wholesale suppliers help sustain long-term parasite control strategies and improve population health outcomes.
Prevention and Public Health Strategies
Preventing intestinal amoebiasis relies heavily on improving sanitation and promoting hygiene. Key preventive measures include:
Ensuring Safe Drinking Water
Boiling or filtering water effectively kills E. histolytica cysts.
Proper Food Handling
Washing fruits and vegetables thoroughly and avoiding street food reduces the risk of ingestion.
Improved Sanitation Infrastructure
Safe waste disposal systems prevent contamination of water sources.
Health Education
Public awareness campaigns can teach communities the importance of handwashing, hygiene, and safe food practices.
Mass Drug Administration (MDA)
Community-wide distribution of antiparasitic drugs often including mebendazole wholesale supplies helps break transmission cycles and improve overall digestive health.
By integrating preventive and treatment strategies, communities can significantly reduce the prevalence and impact of intestinal amoebiasis.
Long-Term Outlook and Global Efforts
The global fight against intestinal amoebiasis requires collaboration between governments, NGOs, and healthcare providers. The World Health Organization (WHO) continues to emphasize sanitation improvements and the availability of essential medications. Access to mebendazole wholesale and other antiparasitic drugs remains a cornerstone of integrated parasite control programs in endemic regions.
Investments in public health infrastructure, improved diagnostic facilities, and educational initiatives will reduce both incidence and recurrence rates. Additionally, research into vaccine development and novel therapies promises new hope for the long-term eradication of amoebiasis and other parasitic diseases affecting digestive health.
Conclusion
Intestinal amoebiasis is more than a transient infection it represents a significant threat to digestive health, particularly in resource-limited regions. The disease disrupts nutrient absorption, damages intestinal integrity, and undermines overall well-being. Effective management requires a combination of accurate diagnosis, targeted drug therapy, and preventive public health measures.
Medications like metronidazole remain central to treatment, while the broader availability of mebendazole wholesale supports community-based programs aimed at controlling multiple parasitic infections. Together, these strategies contribute to better digestive health, improved quality of life, and a stronger foundation for global health equity.